Hydrocortisone 1 Solution for Scalp How Long to Use
See also
Cellulitis & skin infections
Neonatal & infant skin care
Nappy rash
Key points
- Children with eczema require optimal everyday skin management regardless of the appearance of their skin
- Suboptimal everyday skin management is the most common cause of eczema flares and negatively impacts upon a child's quality of life
- It is paramount that caregivers are educated on how to provide their child with optimal eczema cares, adhere to daily treatment, use topical medicines correctly, avoid triggers and identify signs of an eczema flare or skin infection
Background
- Eczema is a chronic inflammatory skin disease that affects 30% of children and causes dry, hot, itchy, red skin
- Eczema often develops before 12 months of age. Few children have lifelong eczema (15%). The earlier the eczema is managed the earlier the child may grow out of their eczema
- Infants commonly develop facial, neck, scalp and truncal eczema; older children develop flexural and extensor eczema
- The distribution, severity and irritation caused by eczema may worsen, this is termed an eczema flare
- Educating caregivers about eczema and its management is key in preventing eczema flares. Eczema flares are commonly due to non-adherence to treatment and overheating.
Assessment
Children with eczema have itchy skin plus 3 or more of the following:
- Atopic history: 1st degree relative or personal history
- Dry skin: Within the past year
- Typical rash distribution: History of rashes involving skin creases (antecubital fossae, popliteal fossae, neck, front of ankles, periorbital area)
- Typical age of onset: History of a recurrent rash before the age of 2 years
- Visible eczema: red and rough skin
Other features
- Associated symptoms (reduced sleep, itch, irritability, poor feeding, failure to thrive and developmental delay)
- Identified triggers
- Previous eczema treatments, including frequency of treatments
- Previous skin infections (e.g. MRSA, VZV, HSV, Molluscum contagiosum, coxsackievirus)
- Zinc or Vitamin D deficiencies (rare) may compound eczema severity.
Red flags
- Poor growth, persistent diarrhoea and/or recurrent infections (consider immunodeficiencies)
- Signs of infected eczema (eg crusted, vesicular, satellite, pustular, erosive, tender, scabbed or weeping lesions on eczematous skin)
 |  |  |
| Eczema bacterial infection | Eczema herpeticum | Eczema coxasackium |
Examination
The type and frequency of eczema treatments changes depending on eczema severity and the presence/absence of infection
- A Scoring Atopic Dermatitis (SCORAD) Index Calculator or Patient-Orientated Eczema Measure (POEM) is used to assess severity, where:
| Eczema Grading | Mild | Moderate | Severe |
| SCORAD | <15 | 15-40 | >40 |
| POEM | <25 | 25-50 | >50 |
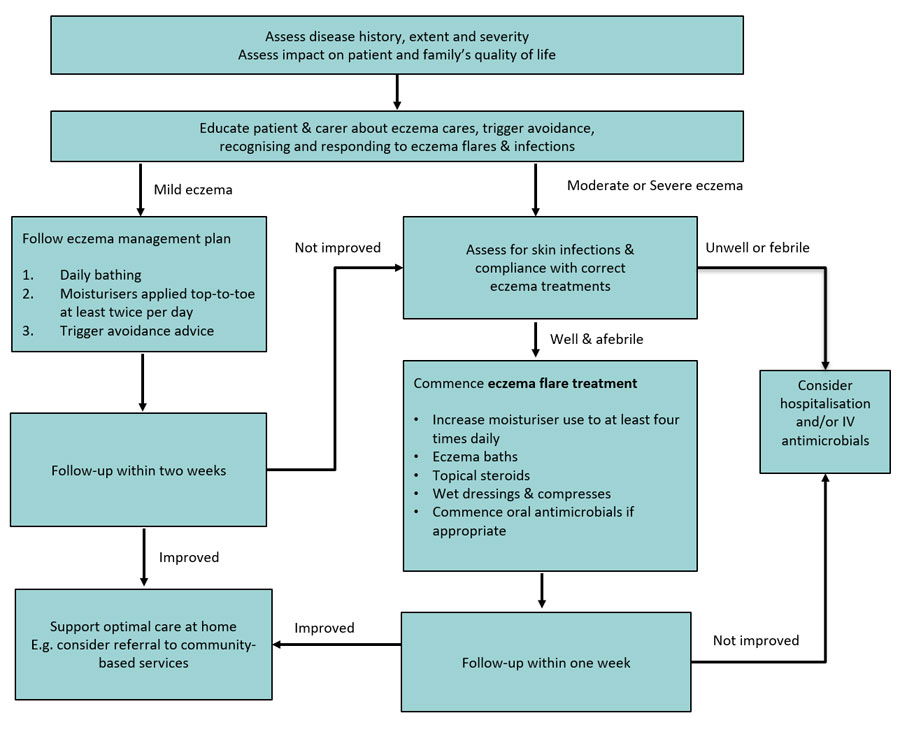
Management
Investigations
- Tests are not required
- If there are concerns of recurrent skin infections or an infection that does not respond to treatment, skin swabs (bacterial or viral) of the lesions may be useful to direct antimicrobial therapy
Treatment
There is no cure for eczema, but it can be well controlled with optimal everyday management and correct treatment of eczema flares.
Common reasons for eczema treatments not being effective include:
- Inadequate education regarding eczema and the correct use of eczema treatments
- Inadequate application of moisturisers, topical steroids and/or wet dressings
- Ongoing exposure to eczema triggers
- Delayed use of eczema flare treatments (e.g. topical steroids and wet dressings)
- Inability to identify and treat skin infections
- MRSA bacterial infection
All children with eczema should be provided with a home eczema management plan and a demonstration of how to correctly apply topical treatments.
Optimal everyday management (clear skin - mild eczema flare, no infection)
In the management of eczema discuss the following with the caregiver.
Children with eczema must bathe daily and have moisturisers applied at least twice per day top-to-toe. This should continue even when the skin is clear.
Moisturisers
- A thick, plain, alcohol-free and fragrance-free moisturiser, with high oil and low water content should be used (see appendix below).
- Avoid contaminating the moisturiser with bacteria from the hands. With tubs use a tool such as a spatula (not hands) to remove it and place it onto clean paper. Moisturiser from the paper can then be applied by hand to the child's skin.
- Apply moisturisers generously twice per day and after bathing or hand washing.
- Avoid moisturisers containing fragrance, plant or food products (eg vegetable, nut or olive oils) as these may disrupt the skin barrier and sensitise the skin leading to food allergies.
Bathing
- Daily bathing aids to reduce the bacterial skin load and reduce the risk of infection
- Baths and showers should be kept luke-warm (<31oC) and limited to 5 minutes to avoid skin flares
- A capful of bath oil should be added to bath water
- Do not use soap or shampoo. Use soap-free skin cleansers that will not irritate the skin
- Use fresh towels with every bath to prevent infections
General considerations
- Keep skin intact: Avoid skin trauma caused by abrasions (eg rough fabrics, sand) and chemicals (eg soaps). Keep fingernails short. Mittens or night-time hand splints may help prevent scratching when asleep.
- Food allergies: Allergy testing is usually not required. As food allergy is not commonly responsible for eczema flares, parents are encouraged to discuss the initiation of restrictive diets with a Dermatologist or General Paediatrician.
- Antihistamines may help ameliorate eczema pruritus. Avoid long-term antihistamine use, manage with eczema flare treatment instead
Minimising common eczema flare triggers
| Overheating | Dry skin | Irritants | Infection/Inflammation |
| Keep baths (<31oC), the home and car cool (<18oC) Avoid air blowing heaters & low humidity environments Avoid thick and multiple layers of clothing | Avoid (alcohol) nappy wipes. Use cloth with water & bath oil. Bathe or shower with bath oil immediately after swimming in a pool Apply barrier cream to the perioral area when the infant is dribbling | Use a non-perfumed clothes detergent Avoid chemicals such as soaps & talcum powders Remove clothing tags Avoid rough & prickly fabrics Manage anxiety or behaviours that promote scratching Keep nail shorts. | Daily bathing using appropriate cleansers and/or bath oils. Wash hands before applying eczema treatments Seek medical review early if concerns of infection not responding to prescribed treatment |
Eczema flares
Steroids:
- Topical steroids (see appendix below) are required once or twice daily until the skin is completely clear to reduce skin inflammation.
- Steroids should be applied generously underneath the moisturiser. Steroid dosage can be calculated using the "Fingertip Unit" method
- Facial eczema should be treated with low potency steroids to avoid chemical skin irritation.
Moisturisers:
- The frequency of moisturiser must increase – apply at least 4 times per day
- Apply the moisturiser on-top of other topical medicines such as steroids.
Wet dressings:
- Assist to return moisture to the skin, protect from infection and further trauma, and help to reduce irritation and itch
- Dressings should be applied with every flare 1-4 times daily for at least 3 days. More frequent dressings and/or longer treatment may be required in severe eczema
- Parents must be educated on how to correctly make and apply wet dressings
- Cool compresses (cloth or towel soaked in water and/or bath oil) should be used on the face or to provide immediate relief of itch before wet dressings
Eczematous skin infections
Broken eczematous skin has a high-risk of bacterial and/or viral skin infections.
Bacterial infections:
- Common causative organisms include Staphylococcus aureus (consider MRSA if no response to first-line antibiotics.)
- Remove crusted lesions by wiping them gently with a cloth whilst soaking in the bath. Only apply topical steroids and moisturisers after the crusts are removed.
- Consider courses of oral antibiotics (eg cefalexin or flucloxacillin for 7 to 10 days).
- Children who are unwell or who have severe infections may require admission and intravenous antibiotics
Viral infections:
- Common causes include coxsackievirus, molluscum contagiosum, herpes simplex and varicella zoster viruses
- Herpetic infection can be treated with antivirals within 72 hours of the onset of symptoms. Intravenous antiviral treatment may be required in severe infections
- Urgent Ophthalmology review is required if the infection extends periorbital (trigeminal) distribution
Recurrent infections:
- Consider patient & family Staphylococcus aureus decolonisation
- Antiseptic preparation may reduce skin bacterial load (eg bleach, benzalkonium chloride, chlorhexidine skin wash, paraffin (OilatumTM bath oil)
Bathing:
- Bleach baths should be used daily with every flare to reduce the bacterial skin load. The addition of salt and oils to the bath also assists in relieving itch and restoring moisture to the skin.
- The child's face and head should be wet during the bath
- Do not rinse after bathing.
Follow up
- Mild eczema: Review with General Practitioner within four weeks
- Moderate to severe eczema:
- Review with General Practitioner within two weeks of starting home eczema management plan.
- Refer to local eczema services (eg Eczema Workshop, Dermatology Nurse Practitioner)
Consider consultation with local paediatric team when:
- Disseminated eczema herpeticum and perioral or severe bacterial eczematous skin infections
- Deterioration of moderate or severe eczema despite compliance with correct treatment(s) for 6 weeks or more
- Severe eczema in a child less than 12 months old
- Poor feeding, poor sleep, failure to thrive
- There is concern that the child's carers are not able to provide appropriate eczema treatments and are unable to access outpatient supports
- Suspicion of concurrent severe allergies (eg recurrent urticarial, systemic flushing, periorbital eczema, eczema limited to exposed skin – limbs)
Staff resources
- Eczema Treatment Plan Generator
- Scoring Atopic Dermatitis Calculator
- Eczema Baths
- Nappy plan sheets
- ASCIA eczema e learns
- Dermatology eczema page
Parent information & resources
- RCH Kids Health Info : Eczema
- Knowing your child's eczema – parent resources page (English, Vietnamese, Mandarin)
- Formula for an eczema bath
- The Eczema Association of Australasia resources
- Eczema and food allergy
Appendix: Medication Information
Encourage families to correctly use liberal amounts of topical skin treatments. Provide children with prescriptions for multiple quantities and repeats (authority) of each medication, to ensure they are always generously applied.
| Type | Example medications | Dosing |
| Bathing oils & wash | QV® bath oil & wash | Use once to twice daily Note do NOT use any bath oils with benzalkonium chloride |
| Moisturisers & Emollients | QV® cream | Apply once or twice daily top-to-toe If eczema flares, apply at least four times per day Barrier creams can be used often when the child is dribbling and applied prior to feeding |
| Topical steroids | For sensitive areas (eg face, nappy)
For body
| Apply once to twice daily to affected areas Ointment are preferred to creams for their emollient effects Lotions are best used for the scalp |
| Antimicrobials | Bacterial infections Viral infections Unwell or severe infection | Only start antiviral infections within 72 hours of onset of infection |
Last updated April 2020
Hydrocortisone 1 Solution for Scalp How Long to Use
Source: https://www.rch.org.au/clinicalguide/guideline_index/eczema/
0 Response to "Hydrocortisone 1 Solution for Scalp How Long to Use"
Post a Comment